Dr. Jessi Gold wants to know, "How do you feel?"
A Q&A about the impact of social media, caregiving, and burnout on our mental health
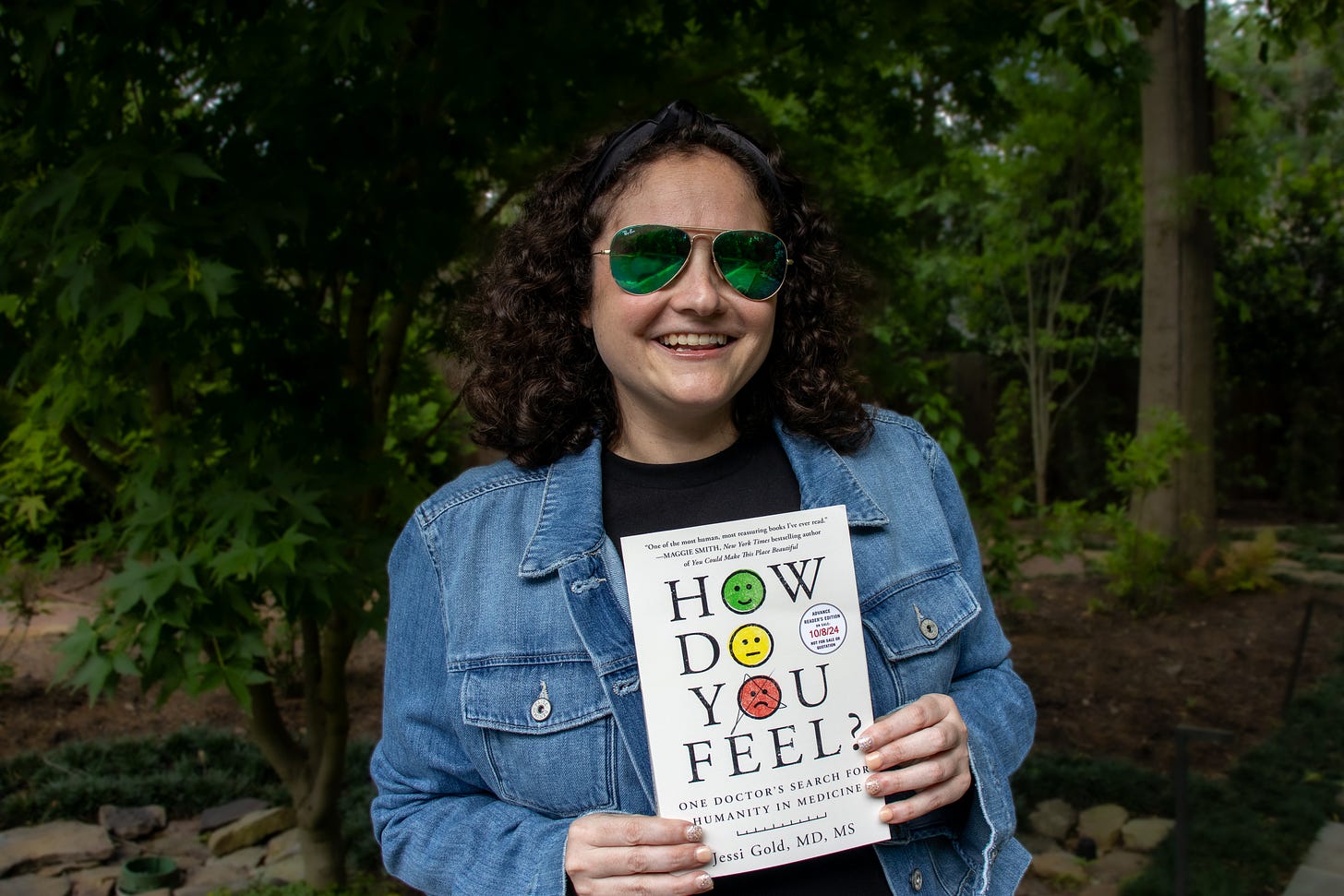
Jessi Gold, MD, MS, is the Chief Wellness Officer of the University of Tennessee System and an associate professor in the Department of Psychiatry at the University of Tennessee Health Science Center, is a fierce mental health advocate and expert. Her first book, “How Do You Feel? One Doctor's Search for Humanity in Medicine” is out now.
Growing up, was mental health a discussed topic in your house?
My dad is a psychiatrist (I’m sure Freud would have something to say about that), and so, growing up I absolutely knew mental health was health, and I knew what it was like for someone to struggle with substances and addiction (his specialty). But, I wouldn’t say my family spent a lot of time talking about our own feelings. It wasn’t actively discouraged, but it also wasn’t modeled. We focused a lot on academics and achievement, and not so much on how it all made us feel. The messages I received from school and home, and simply by watching my three older siblings at school, were really that big emotions got in the way of achievement and being perfect, and I needed to learn to control mine to achieve at a high level. It took me until long after my psychiatry residency training to recognize that it was healthy to be both emotional and ambitious.
What’s your focus area and how did you chose it?
My expertise in psychiatry is in healthcare workers and college students. Both populations have substantial mental health needs, but are often dismissed as “high functioning” or “healthy.” But just because you can still go to school and work, that doesn’t mean you’re actually well. My personal experience is one reason I was drawn to help these groups. When I was in college, I was depressed, and it took a lot for me to go to a therapist and ask for help. I struggled with what so many of my patients do; a “but my grades are good” mentality. I had good grades, sure, but I only wore sweatpants, got takeout, was mostly isolated, and preferred sleeping to everything else. Still, it wasn’t until I stopped going to some of my classes that friends said they were concerned that I agreed to talk to someone.
I wish that were the end of my story, and my experience asking for help was excellent, but after I told my story to the college counselor, they told me I wasn’t sick enough to get care on campus. I felt confused and invalidated, and even though I chose to find another therapist, I learned a lot about mental health in college and the power of a good mental health provider at that key time in someone’s life. I now have the privilege of being a safe landing for my patients, and, at the same time, have the fun job of helping from a systems level, too, as the Chief Wellness Officer for the University of Tennessee System (where I work on wellness broadly, including emotional wellness, for all 5 campuses of the University of Tennessee).
Tell us more about burnout. Is it real?
Burnout, like so many mental health-related words, has become colloquially used incorrectly to mean “work was hard,” and it is so much more than that. It is a very real, workplace-associated constellation of three things:
1) Emotional exhaustion, which can look like physical exhaustion in some people but is really just being spent at the end of the day,
2) Depersonalization or cynicism; feeling disconnected/numb or angry and,
3) A reduced sense of personal accomplishment.
The third one is what most people show up in my office for because that’s when burnout affects achievement. The other two often feel like the consequences of working hard, especially in the US. Just because our workplaces normalize emotional exhaustion and cynicism doesn’t mean that’s healthy. It does make it harder, though, to identify burnout in yourself (“Isn’t this just what working hard feels like?”) and to not blame yourself for somehow not “cutting it” if you choose to get help or take time off for your burnout. I know this first hand—despite being able to rattle off symptoms of burnout in my sleep, I needed my own therapist to name what I was dealing with as burnout. If I struggled to identify it, I think almost everyone does.
How has social media complicated, or maybe even helped, the conversations around mental health?
I’m not anti-social media, but I believe more in the dialectic—that it can be both good AND bad. For mental health, especially through self disclosures and normalizing diagnoses, social media has helped people feel less alone and feel able to talk about otherwise challenging topics. But, with increased “therapy speak” (using mental health terminology without necessarily the proper context or definition), sometimes there is misinformation, misdiagnosis, or overpathologizing of just simply having big feelings. Overall, I think talking about mental health through social media has improved stigma, but I don’t always see that translate to care seeking, especially in psychiatry. Just because you know depression exists, and don’t judge yourself for feeling depressed, that doesn’t mean you will feel comfortable getting treatment for it. You might also still have strong negative beliefs (easy to find on social) about medications, and that could prevent you from seeing someone like me. You might instead look for solutions online and the algorithm will keep showing them to you. But, you can’t supplement or exercise your way out of a severe depression.
Social media also has mixed data on its impact on mental health in general—which is a very popular conversation these days. As someone who sees college students, I'd love the answer to why they have such high mental health needs to simply be social media, but nothing is that simple. Plus, the data is not that good or clear cut. Some researchers note benefits in social as a community or for social anxiety, while others find it affects self-esteem, body image, and mood. I mostly believe we should be more mindful consumers of it and not just passively scroll assuming it impacts us none. If we are on an app, we should regularly pause and notice how the images we are seeing and things we are reading are affecting our mood and body—are you grinding your teeth? Feeling angry? Staying up and not sleeping? If you notice those things, it can be time for a break–and learning how to do that, and mindfully use it, is a skill that I wish we taught and taught early.
Your book is called How Do You Feel? Talk about why you wrote this book and the takeaway for readers.
I was a psychiatrist seeing frontline workers during the pandemic. As I listened, I noticed how many of my patients were struggling with similar things, but felt so alone in their symptoms because it was never talked about, or worse was stigmatized, at work. Having studied and worked with this population long before COVID, I knew it was going to only get worse during and after the pandemic, and felt it was a tipping point to have this conversation and have it publicly. I also burned out pretty badly myself in parallel, and learned a lot about how easy it is to care for others, at the expense of caring for yourself.
Healthcare is just one example of caregiving and we are all better caregivers when we recognize and take care of our own needs. It isn’t selfish, it’s human, and I think seeing me and the patients in the book struggle with that balance is not only validating but enlightening. I hope people who deal with the same universal themes (overwork, perfectionism, empathy, burnout) feel less alone, but also learn some tips and tricks to try in their own lives. It isn’t a self-help book, but readers will see me suggest interventions to my patients and my therapist do the same to me, and can decide if they want to incorporate any of those ideas into their lives. As an added bonus, I hope people can learn that psychiatry isn’t so scary, and it’ll help them know what to expect in our visits, as well as how we think about and do our jobs. Even if it makes one more person recognize their burnout, or less worried about trying a medication, this book did its job.
Connect with Dr. Jessi Gold: Website // Instagram // X
My upcoming book, Fired Up: How to Turn Your Spark Into a Flame and Come Alive at Any Age, is now available for preorder! This book is my guide to figuring out what lights you up and will show you how to live on fire every day. Click here to preorder and get locked into some incredible bonuses.






Important themes. Caring for others brings fragility to the surface. Some of us are never the same again, especially when empathy is at the core. Depression, anxiety, and PTSD are real and can be paralyzing. Interventions, advice, medicine, support, etc. all have tremendous value. The challenge is connecting with those who truly "understand".
Love Dr. Jessi Gold! Thank you for this fabulous interview.