Everything you always wanted to ask another woman about menopause* (*but were afraid to ask)
Covering the waterfront, from horse pee to hair loss
My recent post about my menopause journey generated a lot of conversations and questions on Substack and Instagram; this is my best attempt to answer those questions based on my personal experience and publicly available data.
First, some context: fewer than one in five obstetrics and gynecology residents in America say they received training to treat women going through menopause. A 2019 study found that just 6 percent of residents feel comfortable managing menopause, and over a third said they’re not prepared at all. On average, residents reported having about two hours of menopause education in medical school — TOTAL.
In other words, if you expect your general practitioner or even your ob/gyn to diagnose and treat your menopause, you may be in for a frustrating conversation.
In addition, many doctors — especially the younger ones — have preconceived and even erroneous opinions about prescribing hormone replacement therapy (HRT) to treat menopause symptoms. The New York Times recently published an article recently about why this is the case — in short, a poorly constructed 2002 study and its inaccurate outcomes (which were exaggerated and misconstrued by the media) led many doctors and women to believe HRT is dangerous.
This is problematic for many reasons, but suffice it to say that the 50 million menopausal women in America who have a life expectancy of 85 and will live one-third of their lives after menopause need and deserve care.
Let’s get to your questions:*
How do I know I’m in menopause?
Typically, it’s official when you’ve gone a whole year without a period. That said, only one in five women between the ages of 40 and 60 will receive a menopause diagnosis, even though 80 percent of all women generally experience symptoms. So bring it up with your doctor and if you don’t like their response, find a new doctor!
What labs should I ask for?
“A change in menstrual patterns and the appearance of hot flashes are usually the first signs. Although blood tests are not required, healthcare providers can run blood or urine tests to determine levels of the hormones estradiol, follicle-stimulating hormone, and luteinizing hormone.”
What if my physician won’t even entertain prescribing me HRT?
Get a second opinion. And maybe even a third. You can find doctors who understand menopause and related treatments for symptoms at menopause.org. Here’s more on how to advocate for yourself during your appointment.
The bottom line is that research shows that if you’re within 10 years of menopause and healthy and don’t have any contraindications for HRT — such as a history of stroke, blood clotting, or a known or suspected history of breast cancer — the benefits of HRT very likely outweigh the risks.
Will HRT cause breast cancer?
This is complicated, so consult a doctor who understands the data. But the increase in the risk of breast cancer has been presented this way: “A woman’s risk of having breast cancer between the ages of 50 and 60 is around 2.33 percent. Increasing that risk by 26 percent would mean elevating it to 2.94 percent (smoking, by contrast, increases cancer risk by 2,600 percent). Another way to think about it is that for every 10,000 women who take hormones, an additional eight will develop breast cancer. Avrum Bluming, a co-author of the 2018 book Estrogen Matters, emphasized the importance of putting that risk and others in context. ‘There is a reported risk of pulmonary embolism among postmenopausal women taking estrogen. But what is risk? The risk of embolism is similar to the risk of being on oral contraceptives or being pregnant.’”
Also, consider the risks of not taking HRT: “Heart disease, not cancer, is the leading cause of death for women in every decade of their lives (it is even the leading cause of death for breast cancer survivors). HRT can decrease that risk by 30 percent to 50 percent. It can also cut in half the risk of osteoporotic hip fracture — a crucial benefit because as many older women die annually after breaking a hip as die of breast cancer. And numerous animal and human studies indicate that estrogen is the only intervention that prevents or reduces the risk of Alzheimer’s disease and other forms of dementia in women.” And, “because of estrogen’s benefits for heart, brain and bones, women on HRT live, on average, several years longer than those not taking it. This is one reason that the North American Menopause Society and 30 other international groups concluded that ‘there are no data to support routine discontinuation in women age 65 years.’”
Does HRT cause dementia?
A recent study that caused a flurry of scary headlines is an outlier as scientists could not distinguish the reasons HRT was prescribed to study participants — possibly to treat changes in sleep, mood, memory — from the early symptoms of dementia. Therefore, in some of the women treated with HRT in the study, symptoms that prompted the therapy may actually have reflected early neurological changes. The authors of an editorial published with the report noted the study’s limitations, writing, “The observed associations could be artifactual and should not be used to infer a causal relationship between HRT and dementia risk” or help doctors and patients make decisions about using HRT.
Will HRT cause blood clots?
HRT tablets can increase the risk of blood clots, but the risk is still very low. HRT patches, sprays and gels do not increase the risk of blood clots. This is because estrogen is safer when it's absorbed into your body through your skin.
What were my symptoms?
I was having trouble sleeping (mainly because I was really hot plus frequent peeing in the middle of the night); mood swings; diminished libido; brain fog; joint and muscle pain that began right when my hormone levels dropped due to menopause; tinnitus; hair loss; dry skin and eyes.
Is HRT covered by insurance?
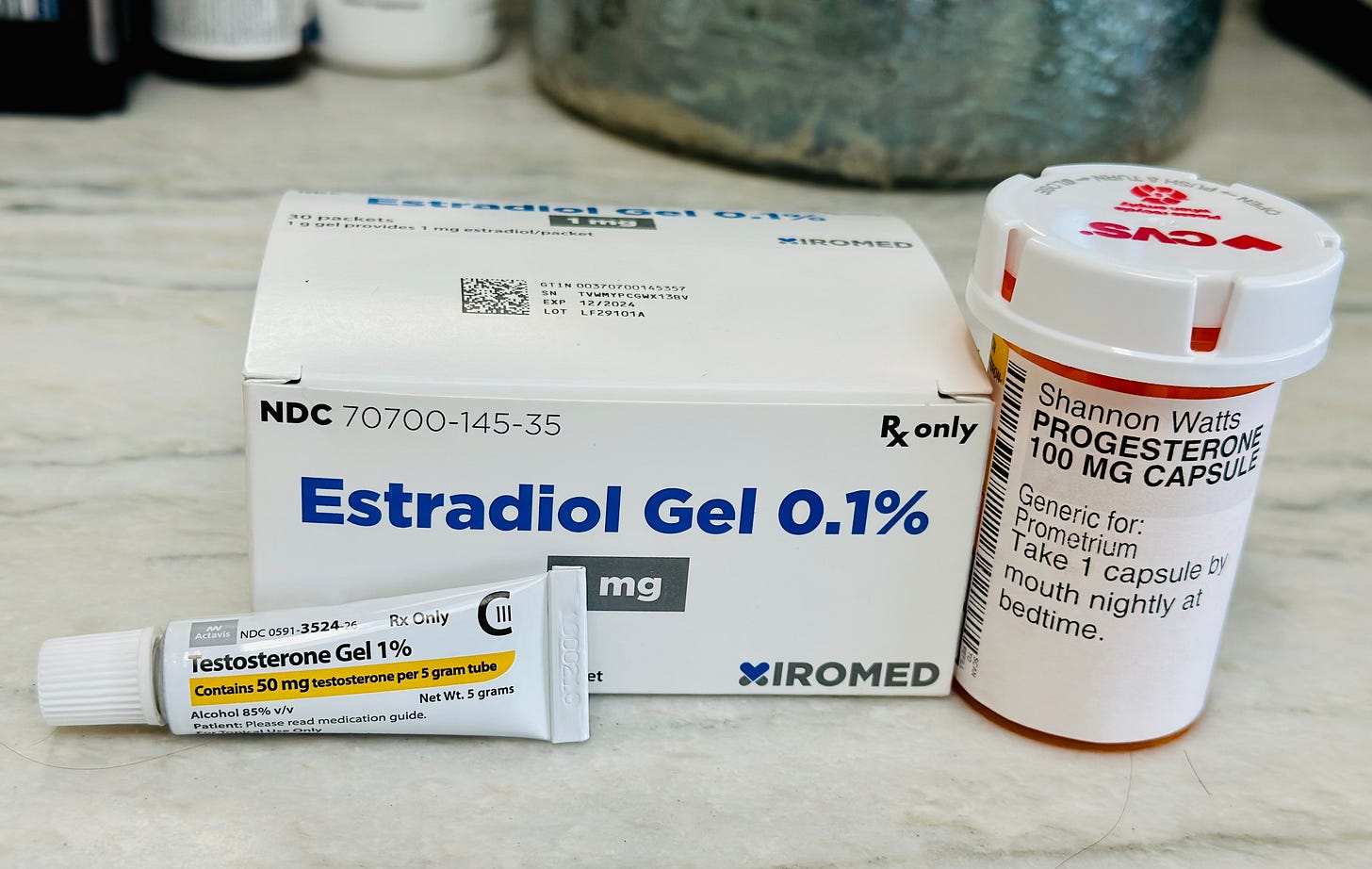
Mine (Cigna) does with the exception of the testosterone, which I pay for out-of-pocket. But the more universal answer is, “it depends.” More than 90 percent of Medicare and Medicaid plans cover estradiol, the most common form of HRT; that figure rises to 99% for commercial insurance plans.
However, having insurance coverage doesn’t necessarily make HRT medications affordable. Although many insurance plans include estradiol products in their formularies, they often place these medications in higher tiers, which have the highest copays. These high out-of-pocket costs are most common with brand-name HRT. Some brand-name HRT treatments have manufacturer discounts that can help you with your copay if you have insurance and the overall cost of the medication whether you have insurance or not.
Also, some insurers draw the line between what they will and will not cover with regard to HRT based on whether the specific therapy is FDA approved. Many bioidentical hormone therapies are not FDA approved and therefore not likely to be covered by insurance.
If your insurance comes through your employer, as your human resources department for information on HRT coverage. Otherwise, call your insurance company directly to ask about the specific types of treatment you’re considering.
Does estrogen contain horse urine?
A kind of oral estrogen called Premarin contains a mixture of multiple estrogens found in the urine of pregnant horses. This type of hormone therapy is typically not used anymore. The estrogen most commonly prescribed is estradiol, which is what the ovary produced before menopause. It’s available in multiple forms, including skin patches, which doctors believe to be safer than taking estrogen orally because it bypasses the liver.
Why does my regimen include testosterone?
My doctor makes it part of the HRT trio he prescribes patients (estrogen, testosterone and progesterone), especially if decreased libido is an issue. Testosterone can also be important in women for bone density and muscle mass, cognitive function, mood and energy. In addition, adequate levels of testosterone are important for the maintenance of musculoskeletal health and possibly even vascular and brain function. Along with estrogen and progesterone, testosterone levels gradually decline during menopause. However, no testosterone products designed for women are on the market or approved by the FDA — in part because long-term studies in women are lacking, including the effects on those who have a history of breast or uterine cancers and liver or cardiovascular disease. Although studies say testosterone is widely used in women, its use is considered off-label.
What if HRT doesn’t help my symptoms?
Well, one thing to consider is what’s up with your pelvic floor, which can be adversely impacted by both childbirth and menopause. ALSO WHY DOES NO ONE TELL US THIS? I have a girlfriend who suffered horribly for years before she finally found a specialist who told she needed two reconstruction surgeries to restore her organs to their original position. Thought exercise: What if men’s organs collapsed inside them? We’d have entire research facilities devoted to preventing and fixing it.
What else do I do personally to treat my menopausal symptoms?
Every couple of months I do a Mona Lisa treatment, a totally painless vaginal laser that allegedly regenerates vaginal tissue. I was pretty excited when my ob/gyn recently told me I have the “vulva vestibule of a 30-year-old” (come to think of it, that needs to go in my Twitter bio).
Heavy weight lifting every day: Two days of legs, two days of arms, one day of core — repeat. I also try to get 7,500 steps in every day. I love an after dinner walk.
I’m trying to be better about yoga for balance, hanging for grip strength, and stretching for flexibility. When I met Jane Fonda she told me she has a physical therapist to help her keep her neck flexible so she can keep driving, including backing out of the driveway. Brilliant!
I try to eat as many grams of protein as I weigh every day. This is very hard to do! But my goal is to help build muscle so I can keep lifting groceries and, eventually, grandkids.
Every morning I take a probiotic, fish oil supplement, general vitamin and extra vitamin D & K. At night, I take magnesium at around 9 pm — I find it helps with restless leg syndrome and sleep. Some research shows it can also help with anxiety. And then before bed I take Ashwagandha, my progesterone prescription, and one of these CBD capsules.
Other helpful resources:
Estrogen Matters book; here it is all summarized in a podcast
This brilliant New York Times article
*(Obviously consult a physician for more accurate and personalized medical advice — and tell them a really pissed off Gen X-er sent you.)





As I read this, I'm literally sweating out a hot flash. 🥵 I've been putting off talking to my doctor for way too long. Thanks for this nudge.
Thank you for continuing this conversation.
A few things I have learned.
1. Dr. Jen Gunther is the expert I look to for information regarding perimenopause and menopause.
2. Go get her book The Menopause Manifesto. It is a comprehensive manual about what the heck is going on with our bodies and the risks and benefits of all the different modalities that we can use to help us.
3. Look for an OB/GYN who is certified by the North American Menopause Society. They have the added certifications, training and expertise to help us.
4. Be weary of MLM scams and MDs who are selling the "magic cure." I know of MDs who sell Plexus and other untested herbal nonsense to their patients. This is unethical and a conflict of interest. They know we are desperate and vulnerable. Don't get sucked in!
Ladies, keep pushing for information and help. Talk about menopause with your friends, mothers and daughters. Also, do not let an MD "poo poo" your symptoms. If they do call them out and if they still do not help you get another provider.